Infertility can be a deeply challenging experience for couples and individuals trying to conceive. While many cases of infertility are treated with standard in vitro fertilization (IVF), severe infertility issues, especially male infertility, often require more specialized approaches. One such treatment is Intracytoplasmic Sperm Hypodermic injection (ICSI), an incredibly advanced fertility technique that has revolutionized the way doctors approach severe infertility. This blog explores the medical and emotional facets of ICSI, shedding light on its importance in treating severe infertility cases and offering information into the experiences of those who undergo botox cosmetic injections.
What is ICSI?
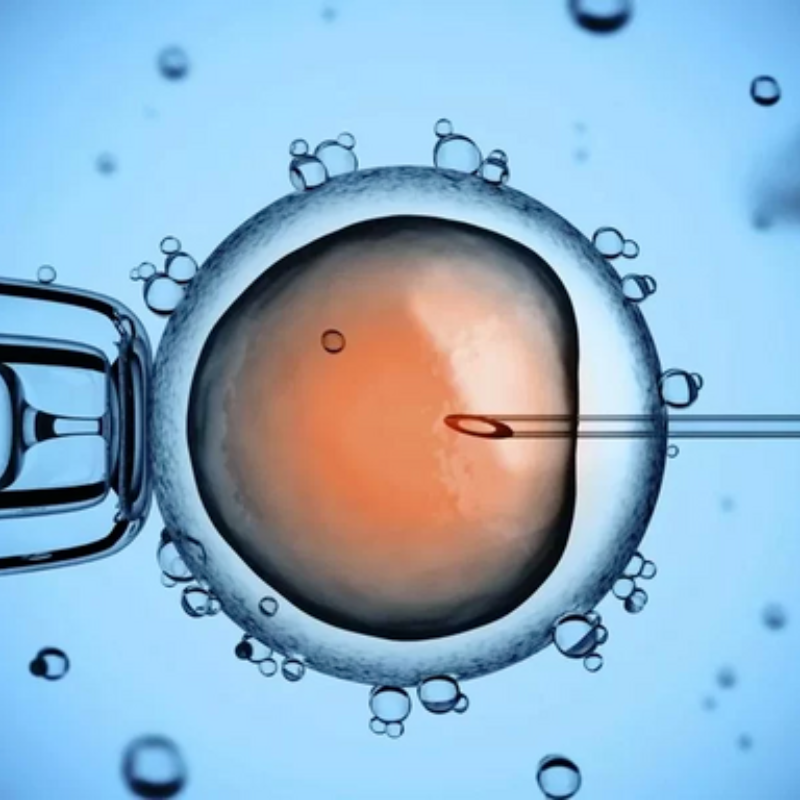
ICSI stands for Intracytoplasmic Sperm Hypodermic injection, an operation when a single sperm cell is being injected straight into an egg cell during an IVF cycle. This ICSI advanced technique is used primarily when male infertility is a significant factor. In traditional IVF, sperm is defined in a petri dish with the offspring and allowed to fertilize naturally. However, in cases of low sperm count, poor sperm motility, or other male fertility issues, fertilization may not occur effectively. ICSI bypasses these challenges by hand injecting sperm into the egg cell, ensuring fertilization even when sperm quality is poor.
The Medical Advancements Behind ICSI
ICSI was initially developed in the early 1990s, and its affect fertility treatment has been unique. Before the advent of ICSI, severe male infertility was normally a roadblock to achieving pregnancy. Today, ICSI is a common and successful treatment for many couples struggling with male infertility. The technique allows for the use of sperm from even the most challenging cases, including sperm with low motility, low count, or poor morphology. Furthermore, ICSI has expanded the number of choices of fertility treatments for men who previously may not have had viable methods of neurological being a parent.
Medical Signals for ICSI
Male Infertility Factors
The primary medical reason for using ICSI is male infertility. This can include various conditions, such as:
Low sperm count (oligospermia): When the number of sperm is insufficient for natural fertilization.
Poor sperm motility (asthenozoospermia): When sperm struggles to frolic in the water effectively, preventing it from reaching and fertilizing the egg cell.
Abnormal sperm morphology (teratozoospermia): When sperm have an unusual shape that limits their capacity to sink into the egg cell.
Sperm obstructions or absence: When a man has a blockage preventing sperm from being ejaculated, or when there is no sperm in the seminal fluid (azoospermia), sperm can be recovered surgically for ICSI.
Female Infertility Factors
While ICSI is typically associated with male infertility, it can also be helpful when female infertility factors exist. For example, women with conditions such as polycystic ovary affliction (PCOS) may benefit from ICSI if traditional IVF methods haven’t succeeded. ICSI is also an option for girls who have experienced multiple failed IVF series or have egg cell quality conditions that may prevent fertilization.
The ICSI Procedure: A Step-by-Step Guide
Ovarian Stimulation and Egg cell Access
The first stage of an ICSI cycle is ovarian stimulation, where the woman experiences hormone therapy to encourage her ovaries to produce multiple offspring. These offspring are then recovered in a minor surgical treatment called egg cell access. The offspring are carefully collected and prepared for fertilization.
Sperm Collection and Preparation
The next step involves collecting sperm from the male partner. When sperm cannot be collected via ejaculation, a surgical treatment may be necessary to retrieve sperm directly from the testicles or epididymis. Once collected, the sperm is carefully prepared in the research laboratory. This includes selecting the healthiest sperm for the ICSI procedure.
Sperm Hypodermic injection into the Egg cell
The most critical the main ICSI procedure involves injecting a single sperm straight into each egg cell using a fine hook. The egg cell is then administered for fertilization, which is confirmed within a period of time.
Embryo Culture and Transfer
Once fertilization occurs, the embryos are cultured for a few days. Typically, doctors strive for day 3 or day 5 embryo transfer, depending on the quality and development of the embryos. The best-quality embryos are selected for transfer to the woman’s uterus, where implantation and pregnancy may occur.
Success Rates and Considerations
Success Rates of ICSI
ICSI has significantly improved the probability of pregnancy for couples facing severe infertility. The success rates of ICSI vary depending on various factors, including the woman’s age, the standard of the offspring, the sperm quality, and any underlying medical ailments. Generally, ICSI has shown success rates much like traditional IVF, with pregnancy rates of around 30-40% per cycle for girls under 35. However, it’s important to note that success rates may decline with maternal age and other factors.
Risks and Considerations
While ICSI is a relatively safe procedure, it is not without its risks. Some of the potential risks include:
Multiple child birth: Due to the transfer greater than one embryo, there is an increased risk of multiple child birth (twins, triplets, etc. ).
Ovarian hyperstimulation affliction (OHSS): In rare cases, the woman’s ovaries could become overstimulated by the the body’s hormones, leading to swelling and discomfort.
Ancestral conditions: There is a slightly increased risk of passing on ancestral conditions due to the use of sperm with potential abnormalities. Pre-implantation ancestral testing (PGT) can be used to reduce this risk.
Despite these risks, ICSI has provided many couples with the chance to become parents when they otherwise might possibly not have had that chance.
The Emotional Impact of ICSI on Couples
The Emotional Rollercoaster of Infertility
The emotional toll of infertility can be unique, and for many couples, the street to being a parent is long and filled with disappointment. ICSI, while offering a potential solution to severe infertility, does not guarantee success. The process can bring a mixture of hope and anxiety, with each stage of treatment carrying its set of emotional challenges.
For couples going through ICSI, the experience can be both exciting and stressful. The emotional altitudes of successful fertilization and the potential for pregnancy are tempered by the anxiety about failure, the tension of multiple treatment series, and the uncertainty of the outcome. Furthermore, the physical demands of the procedure, including hormone treatments and egg cell access, can contribute to emotional and physical fatigue.
Coping with the Emotional Challenges
It’s crucial for couples going through ICSI to acknowledge and address the emotional impact of the treatment. Support from medical experts, fertility therapists, and support groups can help individuals navigate the emotional challenges associated with infertility. Couples should be encouraged to communicate freely, manage expectations, and seek emotional support throughout the process. Many couples also benefit from mindfulness practices, therapy, and stress-relieving activities to face the emotional strain.
The Role of Partner Support
For many couples, the ICSI journey requires a great deal of patience and emotional resilience. Support from a partner is essential during this time period, as it provides emotional strength needed to endure the ups and downs of fertility treatment. Sharing the experience, the wonder and the sorrows, can strengthen the bond between partners, offering comfort during difficult moments.
The Long-Term Emotional Effects of ICSI
Even with a successful pregnancy, the emotional journey doesn’t always end. Couples may experience combining relief, joy, and gratitude alongside anxiety and worry. The anxiety of the process can carry over into the pregnancy and being a parent levels. It’s necessary for couples to maintain emotional support systems after pregnancy to help them navigate any lurking fears or concerns.
Conclusion: A Positive Way to Being a parent
ICSI has revolutionized treating severe infertility, particularly male infertility, providing anticipate to many couples who may have otherwise been unable to conceive. The procedure’s capacity to bypass barriers such as low sperm count or poor motility has transformed the fertility landscape, making being a parent a reality for many. However, the emotional and medical facets of ICSI must be carefully considered. The journey through infertility treatment is often long and emotionally difficult, and couples should seek out support at every step.